Meningitis (Meningococcal invasive disease)
Definition
Meningitis is a general term describing an inflammation around the membranes (meninges) surrounding the brain. Most cases of meningitis are caused by a viral infection, but bacterial and fungal infections can also occur. Meningitis can resolve on its own in a couple of weeks or can become a life-threatening emergency.
The life-threatening disease known as meningococcal invasive disease is what this document focuses on. Meningococcal disease is an illness caused by the bacteria Neisseria meningitidis which causes inflammation of the tissue surrounding the brain and spinal cord (the meninges) resulting in meningitis. N. meningitidis can also infect the blood causing meningococcemia, or the lungs which causes pneumonia.
N. meningitidis is found in the noses and throats of 5 to 10 percent of the normal human population and rarely causes serious disease. However, the bacterium can get through the mucous membranes of the nose and throat and spread throughout the body causing meningococcal “invasive” disease.
Meningococcal invasive disease is reportable to the Iowa Department of Public Health by Iowa Administrative Code 641 IAC 1 .
Symptoms
The symptoms of bacterial meningitis can appear quickly or over several days. Typically they develop within 3 to 4 days after exposure but can range from 2 to 10 days. Symptoms include:
- Fever
- Headache
- Stiff neck
Infants younger than one month old are at a higher risk for severe infection. In newborns and infants, the classic symptoms of fever, headache, and neck stiffness may be absent or difficult to notice. The infant may appear to be slow or inactive, irritable, vomiting or feeding poorly. In young children, doctors may also look at the child’s reflexes, which can also be a sign of meningitis.
Although the early symptoms of viral meningitis and bacterial meningitis may be similar, later symptoms of bacterial meningitis can be very severe (e.g., seizures, coma). For this reason, if you think you or someone else may have meningitis, see a physician as soon as possible.
Symptoms of meningococcemia may include fever, fatigue, vomiting, cold hands and feet, cold chills, severe aches or pain in the muscles, joints, chest or abdomen, rapid breathing, diarrhea - and, in the later stages, a puerperal rash or a petechial rash.
Meningococcal disease caused by any serogroup is very serious. Approximately 10 to 15 percent of people with meningococcal disease die even with appropriate treatment. Of those who recover, up to 20 percent suffer from serious after-effects, such as permanent hearing loss, limb loss, or brain damage. Meningococcal vaccines are very safe and effective at preventing meningococcal disease. The meningococcal vaccine is 85 to 100 percent effective at preventing infection from the subtypes of meningococcus found in the vaccine.
Causes
Meningococcal invasive disease is caused by the bacterium Neisseria meningitides. This bacterium is not as contagious as the common cold or influenza but it can be spread by simply breathing the same air where an infected person has been. The disease typically spreads among people through the exchange of saliva and other respiratory secretions through activities such as kissing, coughing and chewing on toys.
Risk Factors
People in close contact with infected individuals have a higher risk of becoming infected. Viral infections, crowded living conditions, chronic illnesses, and smoking increase a person’s chances of getting the disease. College freshmen, especially those living in crowded residence halls, have shown a higher rate of infection.
Prevention
A meningococcal vaccine is available. There are 13 types of N. meningitidis, nine of which cause invasive disease. The vaccine protects against disease caused by types A, C, Y and W-135 and is recommended for all persons 11 to 18 years of age. Vaccination is recommended for adults if you
- Are a college freshman living in a dormitory
- Are a military recruit
- Have a damaged spleen or your spleen has been removed
- Have terminal complement deficiency
- Are a microbiologist who is routinely exposed to Neisseria meningitidis (the causal pathogen)
- Are traveling to or residing in countries in which the disease is common
For more information on the meningococcal vaccine, visit the CDC’s meningococcal vaccination page.
People should also observe the following precautions to help prevent infection with meningococcal disease:
- Stop smoking
- Avoid other who smoke and keep children out of rooms where others are smoking
- Prevent upper and lower respiratory tract infections by receiving the influenza vaccine (and possibly the pneumococcal vaccine if it is recommended for you)
- Avoid others who are coughing or have colds
People in close contact with infected individuals less than seven days before the person began showing symptoms and while the person is showing symptoms should receive prophylactic antibiotic treatment as soon as possible after exposure.
New meningococcal vaccine requirement for 2017-2018 school year
Beginning in January of 2017, students enrolling in 7th and 12th grades are required to have the meningococcal (A, C, W, Y) vaccine. This will be fully implemented at the beginning of the 2017-2018 school year. This change requires a one-time dose of meningococcal (A, C, W, Y) vaccine received on or after 10 years of age for applicants in grades 7 and above, if born after September 15, 2004; and 2 doses of meningococcal (A, C, W, Y) vaccines for applicants in grade 12, if born after September 15, 1999; or 1 dose if received when applicants are 16 years of age or older. For more information,visit www.idph.iowa.gov/immtb/immunization/laws.
Treatment
Meningococcal disease often requires hospitalization and intravenous administration of antibiotics. Anyone who suspects they may be suffering from this disease should seek immediate treatment from their health care provider. Without treatment, most people infected with meningococcal invasive disease will die.
People who are identified as close contacts to a person with meningococcal invasive disease should receive antibiotics as soon as possible.
Specimen Collection
Optimally, clinical specimens should be obtained before antimicrobial therapy commences in order to avoid loss of viability. Treatment of the patient, however, should not be delayed while awaiting collection of specimens, and a specimen should be obtained in all suspect cases as bacterial pathogens can still be detected even after antimicrobial therapy has begun.
The State Hygienic Laboratory will confirm and serogroup isolates of N. meningitidis. Laboratories are required to submit all isolates cultured from normally sterile sites for serogrouping. This serogrouping aids in public health surveillance and prevention of transmission. In addition, SHL will isolate the organism from appropriate clinical samples upon request.
For more information on submitting specimens, contact SHL at (319) 335-4500, or visit: www.shl.uiowa.edu/
For information on collection and transport of clinical specimens, visit https://www.cdc.gov/meningitis/lab-manual/chpt05-collect-transport-specimens.html.
Note: Isolates obtained from sputum or throat cultures are not considered to come from sterile sites; therefore N. meningitidis from these sites is in itself not indicative of invasive disease and is not reportable. If a patient with culture-positive sputum has an illness compatible with invasive meningococcal disease, this should be reported and the appropriate sterile sites should then be cultured.
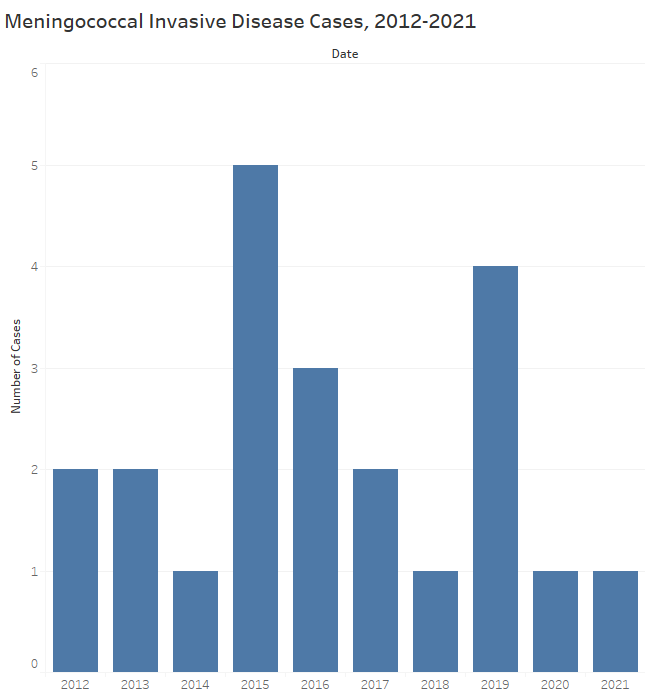
Statistics
In 2021, there was one case of meningococcal invasive disease reported in Iowa.
For more detailed information and statistics on all notifiable diseases, please see our current annual repoort located in the reports section of the CADE homepage.
Additional Resources
Public
Public Health
Schools
Business and Childcare
Health Care Providers